TRIP TO THE DOCTOR
Will psychedelics help Nantucket’s mental health crisis?
story by Robert Cocuzzo
In the fight against mental illness, many believe that psychedelics offer the most promising new forms of treatment. Once rejected as dangerous drugs, psychedelic compounds such as psilocybin (commonly known as “magic mushrooms”), MDMA (commonly known as “ecstasy”) and LSD (commonly known as “acid”) have been shown to have miraculous outcomes in treating severe clinical depression, post-traumatic stress disorder (PTSD), addiction, obsessive-compulsive disorder, eating disorders and other forms of drug-resistant mental illness. So much so that the decriminalization of these substances is opening the door to entirely new therapy practices and practitioners around the country. With the island community continuing to struggle with mental illness, when will these treatments be available on Nantucket? Or are they already here?
“I have seen discussions about these drugs, but I think it would be premature to recommend them until more research is done,” indicated Dr. Timothy Lepore, Nantucket Cottage Hospital’s medical director and chief of surgery who also runs a suboxone clinic treating addiction on the island. “Medical aphorism: Don’t be the first or last to use a medication.” However, Lepore is open-minded about the potential of unconventional treatments. “I have tried low-dose ketamine in a few patients, nasal dose,” he added. “There is evidence it works for depression.”

Originally developed in the 1960s as anesthesia for animals, ketamine was approved by the Food and Drug Administration (FDA) in March 2019 in the form a nasal spray to treat drug-resistant depression and suicidality. “This is a gamechanger,” said Dr. John Krystal of Yale School of Medicine who helped pioneer the research that expedited FDA approval. “With most medications, like Valium, the anti-anxiety effect you get only lasts when it is in your system. When the Valium goes away, you can get rebound anxiety. When you take ketamine, it triggers reactions in your cortex that enable brain connections to regrow. It’s the reaction to ketamine, not the presence of ketamine in the body that constitutes its effects.”

While the FDA has paved the way for ketamine clinics to pop up throughout the country where doctors can legally administer the drug to patients, those seeking treatments by way of illegal substances such as psilocybin have had to seek out “underground guides.” With their cultivation stemming back to shamans in Mexico, magic mushrooms were first popularized in the United States by Life magazine after a banker turned amateur mycologist named R. Gordon Wasson became one of the first Westerners to participate in a mushroom ritual in Oaxaca, Mexico, in 1955. Wasson wrote about his experience in an eight-page photo essay titled “Seeking the Magic Mushroom” that was read by millions of Americans. A version of this tradition of shamans or guides that Wasson encountered in Mexico has quietly flourished in the United States with a network of practitioners treating patients with some of the same ancient rituals.
One man in his late thirties, who asked to remain anonymous, described his experience of a therapeutic psilocybin journey administered by an underground guide off island. “I had been battling bouts of depression since the age of eighteen,” he said. “I’d been seeing therapists for years and had been taking two different antidepressants as the result of a major clinical depression.” After becoming frustrated with the lack of reprieve and progress he found with the antidepressants, the man was put in touch with an underground guide by friends. Following a series of onboarding sessions in which he and the guide discussed his intentions for the journey, the man spent a day consuming higher and higher doses of psilocybin administered in the form of a tea from the guide.
“There were some very hard and intense moments during the journey,” he reflected. “But I was ultimately able to experience a new perspective—not just see it, but feel it—and something deep shifted within me.” Following the day-long session, he returned to the guide to discuss how to integrate the takeaways from his journey thereafter. Today, the man reports being completely off of all antidepressants with no symptoms of depression. “It was nothing short of life-changing.”
In recent years, at least one shaman has come to Nantucket to preside over underground group ceremonies held in a private residence where ayahuasca and peyote were administered over the course of two nights. Speaking under the condition of anonymity, a participant of one of these private ceremonies described a rigorous pre-interview with the shaman during which she voiced her intentions for the psychedelic journey. She arrived on the first night of the ceremony wearing all white, as each participant was instructed to do, and encountered many familiar faces from around the community. After a series of rituals, the participants consumed ayahuasca tea and then were shown to a mat where they would lie down for that night’s inner voyage. The following morning, they consumed peyote followed by another nighttime session with ayahuasca.


Reflecting on the impact of each session, the participant spoke glowingly of the transformation and healing she experienced. Her deep, long-held psychological pain was released and she found lasting inner peace. Although she considers the experience overwhelmingly positive, the participant was troubled by some aspects of the ceremony in retrospect, specifically the number of people who ultimately became involved. What she had originally thought was only going to be seven participants turned into around twenty by the second night. Her concern was that there were too many people in the throes of an intense psychedelic trip for one shaman and an assistant to care for at once.
In his widely viewed Netflix documentary Have a Good Trip: Adventures in Psychedelics, Nantucket-native Donick Cary featured dozens of famous actors, musicians, comedians and other public figures discussing their experiences with psychedelics. Cary is now in the process of producing a sequel to the film that hones in on the therapeutic advances being made with these compounds.
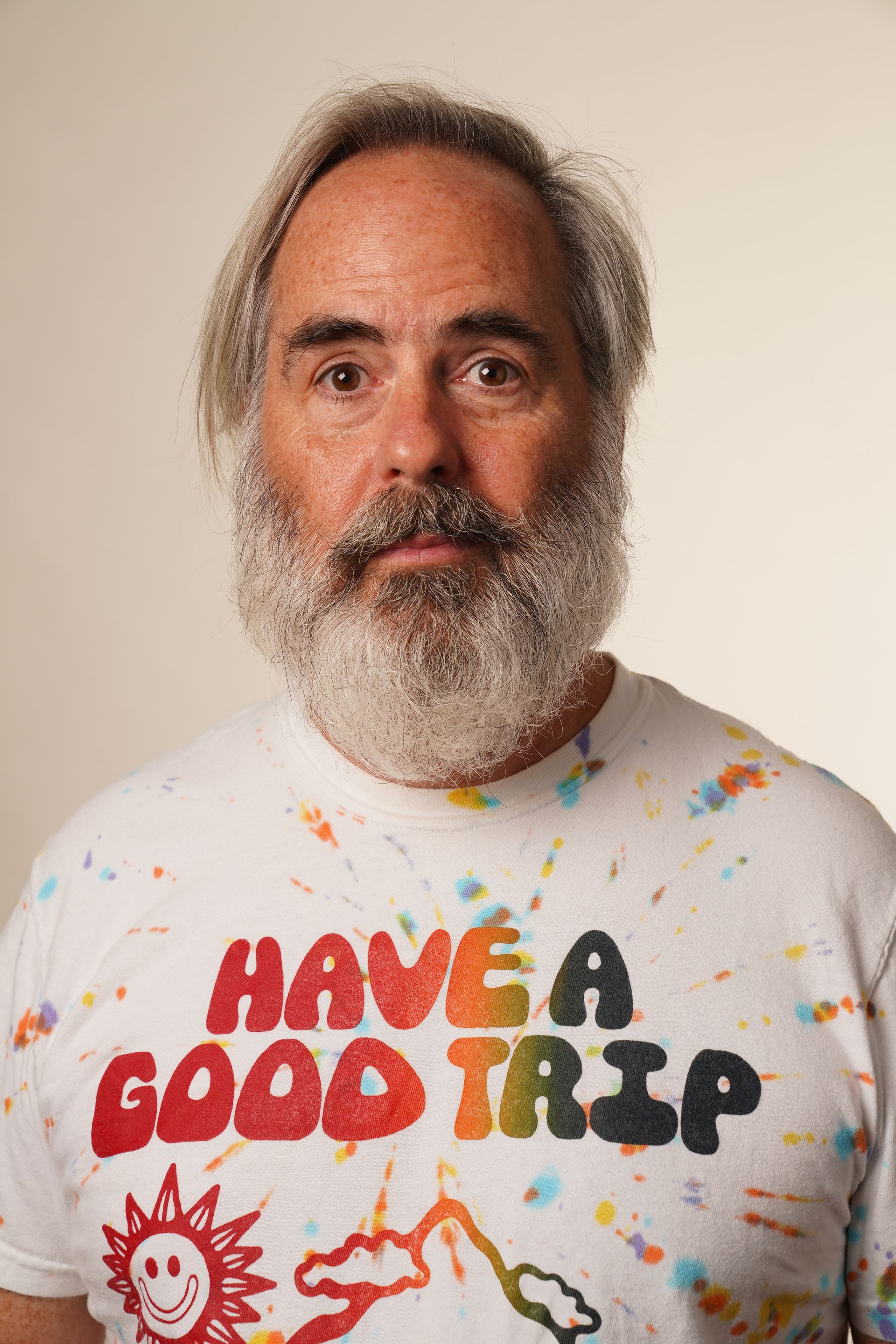
“Part of what we lost over the last fifty years by having psychedelics so stigmatized and becoming part of the war on drugs and becoming something that we were so scared of that we equated it with crack cocaine—we lost fifty years of really looking at how this can help with the mental health crisis we’re in,” he said. “So there’s a lot of stuff we don’t know, which we’re at a moment where there’s a whole bunch of possibilities where we can learn about that, discover that and explore that. But there is stuff that we do know that’s all really positive.”
Cary said that we should stop looking at psychedelics as drugs, but rather as medicines. As these psychedelics continue along the path of decriminalization and become more mainstream, he also advocates a highly careful integration. “My biggest fear is that we as humanity get it wrong, where we say ‘get this stuff out there,’ and we set ourselves up to have horror stories where people who shouldn’t be touching this stuff are taking too much of it and making huge mistakes,” he said. “And these stories scare everyone in Congress, and the war on drugs comes back.”
Massachusetts is uniquely positioned to the advent of these therapies. This past January, lawmakers filed two bills to decriminalize psychedelics like psilocybin, mescaline and MDMA statewide on the basis of their dramatic therapeutic potential. The bills, now before the state Senate, come after Somerville became the first community in Massachusetts to decriminalize entheogenic plants possessed by adults. This legislation is bolstered by the fact that one of the global leaders in psychedelic advocacy and education, the Multidisciplinary Association for Psychedelic Studies, commonly referred to as MAPS, has a heavy presence in Boston. In March 2021, Massachusetts General Hospital followed the lead of Johns Hopkins, New York University and UCLA, which have been studying the impact of psychedelics in end-of-life care for years, when it launched the Center for the Neuroscience of Psychedelics to study “how psychedelics enhance the brain’s capacity for change, to optimize current treatments and create new treatments for mental illness, and to make the term ‘treatment resistant’ obsolete.”
With all this happening, how is Nantucket preparing for the possibility of these treatments? “At Fairwinds, we are attending very closely to developments in this area but do not anticipate implementing these programs in the near future until data on safety and long-term effects are developed,” said David Barlow, Ph.D, ABPP, a board director and Clinical Committee chair at Fairwinds, Nantucket’s Counseling Center. “In the meantime, unfortunately, these drugs have been in use illegally for years often with tragic consequences, including psychotic breaks and deaths, particularly for those with existing mental disorders.”
That is not to say that Barlow and his contemporaries at Fairwinds do not acknowledge the tremendous potential of these treatments, citing that “ketamine and psilocybin and sometimes LSD are beginning to show some promise, particularly for treatment-resistant depression [deep depression that has not responded to an adequate course of antidepressant medications or cognitive behavioral therapy] as well as PTSD.” But as Dr. Dominic Maxwell, the medical director of Fairwinds, put it, “These treatments remain the subject of intensive ongoing research, and while we are hopeful that they may one day be added to our collection of tools to tackle various psychiatric conditions, for the time being we simply do not have the necessary evidence or data to advocate for their use.”
Among mental health professionals, there remains significant trepidation around even addressing these unconventional treatments. When asked for its position on the potential use of psychedelics, Gosnold, a national mental health organization treating patients on Nantucket, declined to comment, but instead shared a link to studies being done at Massachusetts General Hospital. For some practitioners, this reluctance to address these compounds is frustrating. “We’re really in pretty dire times and we need solutions that work,” said Lauren Taus, a psychotherapist based on the West Coast. “These medicines both scientifically and spiritually work to get people results that they might never get in a lifetime of pursuing help.” Taus, who treats patients with ketamine, has witnessed this firsthand. After nine years of treating patients as a therapist, Taus began integrating psychedelics into her practice four years ago and saw dramatic results. “I’ve seen people go from suicidal despair to thrive,” she said. “There’s no doubt that this is the future of mental health care if we are going to make progress. We have made so much progress in so many other verticals in medicine, but within the realms of mental health, we haven’t. And we’re not OK. We’re just collectively not OK. These are not panaceas; this is not all of a sudden cure anyone. But these interventions, when worked with well, are some of the most effective interventions for some of the most difficult pathological processes known to humans.”







